Monoclonal gammopathies include a wide spectrum of disorders ranging in severity from monoclonal gammopathy of undetermined significance (MGUS) and monoclonal gammopathy of renal significance (MGRS), to active multiple myeloma (MM), amyloid light-chain (AL) amyloidosis and non-Hodgkin lymphoma, among many others [1, 2]. MGUS is a precursor to MM and related diseases [3, 4], and light chain (LC)-MGUS a precursor to LC-MM and AL amyloidosis [5]. In addition to serum protein electrophoresis (SPEP) and serum immunofixation electrophoresis (IFE), the serum free light chain (FLC) assay has become the method of choice for detection, prognostication, and monitoring of monoclonal gammopathies [6]. LC-MGUS is defined as an FLC ratio and involved FLC level outside reference intervals without evidence of end-organ damage, MGUS, or other lymphoproliferative disorders (LP). However, as FLCs are primarily cleared by the kidneys, the kidney function is a major determinant of the serum concentration [7]. The prevalence of LC-MGUS in individuals with chronic kidney disease (CKD) is uncertain.
The Iceland Screens, Treats or Prevents MM (iStopMM) study is a nationwide, prospective screening study were all individuals born in 1975 and earlier were invited for screening with SPEP and FLC with over 80,000 (54%) individuals providing informed consent [13]. Here we estimate the association between absolute FLCs levels and FLC ratio with kidney function in a large prospective population-based cohort. The aim was to establish a kidney reference interval for FLCs, and either confirm the previously reported kidney reference interval for the FLC ratio or propose new reference intervals for patients with CKD.
The study was approved by the National Bioethics Committee and the Data Protection Authority in Iceland. All participants enrolled in the study gave their informed written consent.
The iStopMM study is a nationwide, prospective study with the overall aim to assess the benefits and harms of early detection by screening for MGUS and LC-MGUS (ClinicalTrials.gov number NCT03327597). All residents of Iceland registered on September 9th 2016, born in 1975 or earlier (n = 148,711) were invited to participate in the study, of whom 80,759 (54.3%) gave their written consent. A detailed description of the iStopMM study methods have previously been published [13].
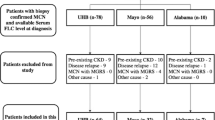
Sera from 75,422 (93%) study participants were obtained and shipped to The Binding Site Ltd. in Birmingham, UK for analysis of SPEP, IFE, and sFLC. All samples were screened for M protein by SPEP using capillary zone electrophoresis (CZE; Helena Laboratories, Texas, USA). IFE (Helena Laboratories, TX, USA) was performed when the CZE was suspicious for M protein bands or when the FLC results based on standard reference intervals were abnormal. Quantification of kappa and lambda FLCs was done using FREELITE TM reagents sets from The Binding Site Ltd. A more detailed description of analytic methods have been published elsewhere [13].
All serum creatinine (SCr) measurements from the participants performed for clinical indications were collected from a central laboratory database. The SCr values were used to calculate eGFR using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [14]. Demographic data and all previous International Classification of Diseases, 9th and 10th revisions (ICD-9 and ICD-10) diagnosis codes were obtained from the Icelandic Directorate of Health for assessment of the participants‘ comorbid conditions, categorized into disease groups for analysis [13]. The accuracy of disease diagnosis in the registry has recently been validated [15]. Information on renal replacement therapy (RRT), i.e. hemodialysis, peritoneal dialysis, and kidney transplantation, was obtained from the Icelandic End-Stage Kidney Disease Registry.
Participants with M protein on IFE or involved/uninvolved sFLC ratio ≥100 with serum involved FLC ≥ 100 mg/L (myeloma defining event) [16], were excluded. The involved FLC was defined as the FLC with the higher absolute concentration. The SCr measurement closest to the screening was used for calculation of eGFR; participants without SCr measurement available within one year before or after screening were excluded. An algorithm based partly on the KDIGO diagnostic criteria for acute kidney injury (AKI) [17], that has been validated [18], was used to detect SCr measurements consistent with an AKI episode. These SCr measurements were excluded, alongside any SCr measurements performed in the ten day period following presumed AKI. This was done to minimize the effect of sudden changes in kidney function on our findings. Participants who were undergoing hemodialysis or peritoneal dialysis or had a transplanted kidney at the time of screening were excluded from main analysis and analyzed seperately. LC-MGUS was defined as an FLC ratio outside the reference interval and an increase in involved FLC without evidence of monoclonal heavy chain on SPEP or IFE, or end-organ damage attributed to the plasma cell proliferative disorder [5].
Normality of data was assessed by direct visualization and the Anderson-Darling test [19]. The 2.5 and 97.5 percentiles of the distributions of kappa FLC, lambda FLC, and FLC ratio were assessed in the whole group, and in subgroups based on age, sex and eGFR representing CKD stages 3–5. A nonparametric bootstrapping method was used to calculate the 95% confidence intervals (CI) for the central 95 and 99 percentile limits. Outliers were assessed using Horn’s algorithm [20] but were not removed from analysis.
The decision on whether a reference interval was partitioned was based on distribution of subgroups (age, sex, eGFR) outside whole group reference interval. If a subgroup distribution outside central 95% reference interval exceeded 4.1% or was below 0.9%, the reference interval was partitioned based on subgroups as recommended by Lahti et al. [21]. A minimum sample size of 120 individuals was used to determine a subgroup reference interval as recommended by joint guidelines from the Clinical and Laboratory Standards Institute and the International Federation of Clinical Chemistry [22]. A sample size of approximately 340 should give an estimate of the population mean with an precision of + /−2%. Central 95% and 99% reference intervals were estimated for serum kappa and lambda FLC, and the FLC ratio for the whole study cohort, and subgroups of age, sex, and eGFR (< 60 mL/min/1.73 m 2 ). A substantial proportion of eGFR subgroup distribution was outside the whole group common reference limits (Supplementary Table IABC). Accordingly, the reference intervals were defined by eGFR categories 45–59, 30–44, and < 30 mL/min/1.73 m 2 for kappa and lambda FLC, and the FLC ratio. A considerable proportion of participants with eGFR < 15 mL/min/1.73 m 2 had values outside the common reference interval, but due to their low number (N = 55), the reference intervals for eGFR < 15 and 15–29 mL/min/1.73 m 2 were combined. After partitioning by these eGFR categories (45–59, 30–44, and < 30 mL/min/1.73 m 2 ), the proportion of age and sex subgroups with levels outside reference intervals were considered appropriate. A sensitivity analysis using only participants with SCr measured at the time of screening was performed.
The revised reference intervals were plotted and compared to currently used reference intervals as well as previously published kidney reference interval of FLC ratio for individuals with reduced kidney function. Correlation between FLC measurements, eGFR and age was assessed graphically and using the Spearman correlation coefficient. Comparison of baseline characteristics and comorbid conditions between groups was carried out using the Chi-square test, the t-test/Wilcoxon rank sum test, analysis of variance/Kruskal– Wallis test, as appropriate.
The prevalence of LC-MGUS in individuals with CKD was assessed both using previously published reference intervals and our proposed reference intervals and the crude rate reported. All statistical analysis and data visualization was performed using R (version 3.6.3).
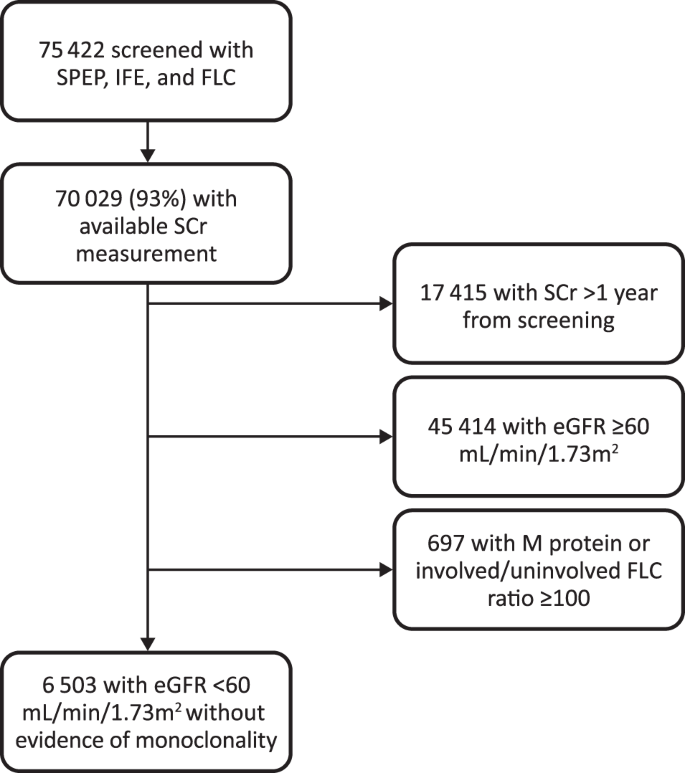
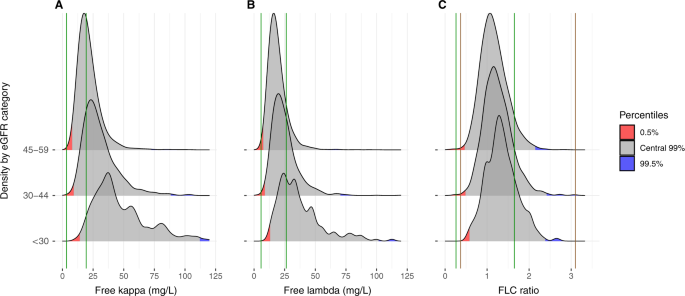
Table 3 Novel reference intervals for serum kappa FLC (mg/L), serum lambda FLC (mg/L), and FLC ratio in individuals with eGFR of 45–59, 30–44, and < 30 mL/min/1.73 m 2 .
Table 4 Comparison of LC-MGUS rates using standard reference intervals and new reference intervals (FLC ratio and kappa, and lambda FLCs) in participants with eGFR < 60 mL/min/1.73 m 2 .
Using data from the population-based, prospective iStopMM screening study, we show that a majority of individuals with CKD and without evidence of monoclonal gammopathy had serum kappa FLC or lambda FLC levels outside current reference intervals. Moreover, while the proportion of participants that had a FLC ratio outside the standard reference interval was too large (9%), the proportion that was outside of the previously published kidney reference interval was low (0.7%). FLC and FLC ratio increased with declining eGFR and increasing age, although age-related increase in FLC levels diminished after taking eGFR into account. We propose new reference intervals for serum kappa and lambda FLC, and the FLC ratio based on kidney function and show that our novel reference intervals performed well in patients on dialysis therapy and in kidney transplant recipients. We suggest adapting these novel kidney reference intervals for assessment of monoclonal gammopathies in individuals with CKD.
Serum kappa and lambda FLC and the FLC ratio increased significantly with worsening kidney function. FLCs are primarily removed by the kidneys and thus kidney function is a major determinant of the serum levels of both kappa and lambda FLCs [23]. Kappa FLCs are formed at approximately twice the rate of lambda FLC in a normal state [24]. Lambda FLCs are more prone to form dimers, increasing their molecular weight and slowing their kidney clearance [7]. With decreasing kidney function, the serum half life of FLCs lengthens which increases the levels of FLCs despite the absence of a pathological plasma cell disorder [7]. This effect is well demonstrated in our study as 9.1% of participants had FLC ratio outside the standard reference interval (0.26–1.65), emphasizing the need for a kidney reference interval. This is comparable to the previous study by Hutchison et al. in a cohort of 688 patients that was used to define the current kidney reference interval for FLC ratio [9]. However, the concentrations of FLCs were much lower in our cohort (median kappa FLC 21.7 vs. 43.8 mg/L and median lambda FLC 19.0 vs. 38.0 mg/L). The reason for discrepancy between the two studies is probably multifactorial and can partly be explained by lower median eGFR (29 vs. 51 mL/min/1.73 m 2 ) in their study, and possibly by different methods for estimating GFR.
Using the previously published kidney reference interval for FLC ratio in our cohort yielded a prevalence rate of LC-MGUS of 0.7%. If the previously published kidney reference intervals were reliable, this would suggests that the prevalence of LC-MGUS is not increased in individuals with CKD [5]. Previous information on the prevalence of LC-MGUS in patients with CKD is limited. Dispenzieri et al. estimated the prevalence of LC-MGUS in a general cohort as 0.8%, but did not include information on kidney function [5]. Fenton et al reported a prevalence of 1.6%, but information on SPEP and IFE results was only available for a small part of their cohort, causing high rate of undetected heavy chain gammopathies [25], but where SPEP was available they reported an increased rate of heavy chain MGUS in patients with CKD [25]. Furthermore, the prevalence of LC-MGUS increased with age which is in agreement with the results of previous research on MGUS among individuals with preserved kidney function [5, 12]. All patients in our study with abnormal FLC ratio based on the aforementioned kidney reference interval also had abnormal FLCs. This differs from previous data on FLC and FLC ratio in the general population where the majority (63%) of persons with abnormal FLC ratio without heavy chain MGUS have normal FLCs [5]. The definition of LC-MGUS requires abnormal levels of both FLC ratio and the involved FLC [16]. Current reference intervals therefore select a different group of individuals with CKD compared with persons with normal kidney function. This indicates that the previously published kidney FLC ratio interval is relatively wide compared to the kappa FLC and lambda FLC reference intervals, resulting in skewed assessment of monoclonal disorders in CKD patients. This notion is important as previous studies on MGUS follow-up, progression, and outcomes are mostly based on data from individuals with normal kidney function [5, 26].
When we used our novel kidney reference intervals, the prevalence of LC-MGUS was 0.5%. The changes in reference intervals therefore caused a relative decrease in the prevalence of LC-MGUS among participants with CKD of 29% compared with previously published kidney reference intervals. The prevalence was lower than previously reported in a general population [5]. This is based on our novel central 99% reference interval, but when the novel central 95% reference interval was used the prevalence increased substantially to 1.2%. We recommend the use of the central 99% reference interval instead of 95% reference interval in clinical practice to decrease the false positive rate of LC-MGUS.
The clinical implications of our findings are substantial. We propose that the novel reference intervals be implemented in clinical practice when assessing serum FLCs in individuals with CKD stage 3 and above. These reference intervals should be used with caution in individuals with acute kidney injury as the SCr and eGFR do not reflect baseline kidney function, and a repeated FLC measurement when kidney function has stabilized is therefore recommended.
A major strength of this study is the large scope of high-quality data. The nationwide population-based cohort comprising 51% of all Icelanders born 1975 or earlier who were screened with SPEP, IFE, and FLC, with all previous SCr measurements available for all participants, allowed us to carry out a meticulous examination of monoclonal gammopathies and accurate assessment of kidney function. All SPEP, IFE, and FLC measurements were performed at the same laboratory using the same methods, thereby decreasing the effect of inter-assay variability. The size of the cohort allowed division of reference intervals into subgroups based on kidney function, yielding more precise determination of the intervals. Furthermore, this study was carried out in a screened population and thus free from selection bias present in other studies.
In conclusion, using data from the iStopMM study comprising a large population-based screened cohort with careful assessment of monoclonal gammopathies and kidney function, we established that current reference intervals for FLC and FLC ratio are inaccurate. Furthermore, we propose new more reliable kidney reference intervals for serum kappa and lambda FLC, and the FLC ratio based on the level of kidney function. Our findings show that these reference intervals also appear to be accurate in individuals on dialysis and in kidney transplant recipients. The novel reference intervals for absolute FLCs are wider and higher than the standard intervals. Furthermore, we suggest narrowing the kidney reference interval for FLC ratio. Implementing the novel reference intervals in clinical practice is likely to increase the utility of the assay for monoclonal gammopathies in individuals with CKD.
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request. The code generated and used during the current study is available from the corresponding author on reasonable request.
Dr. Kristinsson has received research funding from International Myeloma Foundation, European Research Council, Icelandic Center for Research (Rannís), Amgen, Celgene. Dr. Long has received research funding from the Icelandic Center for Research (Rannís). Dr. Landgren thanks Sylvester Comprehensive Cancer Center Core Grant (P30 CA240139) and Paula and Rodger Riney Foundation for support of his research. Dr. Hultcrantz thanks the Memorial Sloan Kettering Cancer Center Core Grant (P30 CA008748). The iStopMM study is funded by the Black Swan Research Initiative by the International Myeloma Foundation, the European Research Council, and the Icelandic Center for Research. Screening tests for the iStopMM study are performed by The Binding Site Ltd. Birmingham, UK. Additional funding is provided by the University of Iceland, Landspitali–The National University Hospital, and the Icelandic Cancer Society.